Education: Oncology Nursing
- Cynthia and Laura Love
- May 1
- 6 min read
May is Oncology Nursing Month. Their theme is Caring Beyond Limits, focusing on their expertise, compassion, and commitment to the patients and families they care for. With cancer being the second leading cause of death in the United States and a significant cause of death worldwide, most nurses will have cared for a patient with this, if not the primary diagnosis, but in their medical history. The word cancer can strike fear in many people when it is spoken. But with advances in treatment options, early detection, and decreased use of tobacco products, the mortality rate declined by 34% from 1991 - 2022 in the U.S. (ACS, 2025).
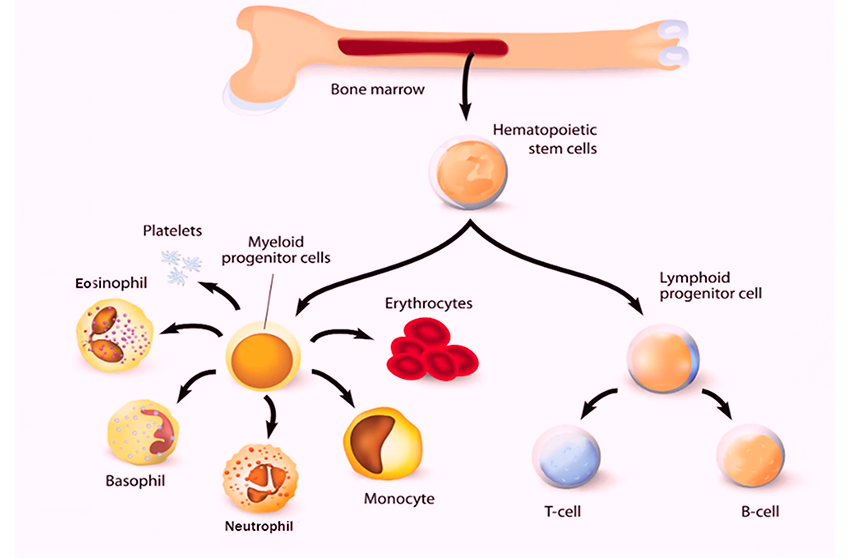
The picture below is a great visual from the American Society of Hematology showing how the hematopoietic stem cells from bone marrow help form red blood cells, white blood cells, and platelets.
(American Society of Hematology, 2025)
Focus on Neutrophils
The most common type of white blood cells (WBC)
It makes up 55% to 70% of the WBC count
First line of defense against infection
Can only live for a short time, research varies on the exact time, but an average is 24 hours
The short lifespan makes transfusions not a viable option
(American Hematological Society, 2025)
Many cancer treatments can often cause a reduction in neutrophils.
This is called neutropenia.
Neutro = neutrophils Penia = deficiency or decrease
Neutropenia
Common Causes
Chemotherapy
Radiation
Cancers that affect the bone marrow, such as leukemias and lymphomas
Common Signs and Symptoms
Low-grade fever (usually 100.40F (380C) for one hour
Odynophagia = painful swallowing
Sore mouth
Body aches
Sore throat
Runny nose
Cough that is new or worsening
Dyspnea
Perirectal pain, irritation, and infection of the genital areas
Assess the catheter site for redness, tenderness, or swelling
Diagnosis
Thorough history and physical
CBC with differential
Absolute Neutrophil Count (ANC)
Looks at the percentage of neutrophils in the WBC count
Average normal range 2500 - 8000/uL
Below 1500/uL increased risk for opportunistic infection
Below 500/uL severely neutropenic
Below 100/uL is extremely high risk for infection due to agranulocytosis (almost no neutrophils in the peripheral blood)
Additional blood work
CMP
Blood Cultures
Folate
Additional diagnostic tests may be run depending on what the provider would like to do
Management
The Provider may discontinue the offending drugs or agents if known
Hand hygiene is crucial
Avoid rectal temps
Avoid constipation, provide stool softeners as needed
Assess skin for any signs of infections, abrasions, and if any, administer prompt care as directed by the Provider
The Provider may order neutropenic isolation
Staff will wear PPE when entering the room
Door will be kept closed to the patient’s room
Visitors may be limited and required to wear PPE
No uncooked meats, fruits, or vegetables
Juices and milk should be pasteurized
Damp dusting to clean rather than dry dusting
No fresh flowers or live plants in the room
Medications
Antibiotics may be used to fight infection or prophylactically if the patient will experience a neutrophil count less than 100uL for more than 7 days
Colony-stimulating factor such as:
Filgrastim/ Brand Name: Neupogen
Pegfilgrastim / Brand Name: Neulasta
Sargramostim / Brand Name: Leukine
(Subhan Waleed et al., 2024)
Neutropenic Patient Education: A Guide for Nurses
Educating neutropenic patients and their families is critical to care, directly impacting patient outcomes and survival. Nurses must be thorough and consistent in providing and reinforcing education throughout hospitalization. Ongoing teaching ensures comprehension, promotes self-advocacy, and reinforces key principles of infection prevention.
Key Education Areas for the Neutropenic Patient
1. Monitoring for Signs of Infection
Early identification of infection is vital. Teach patients and caregivers to recognize and report the following:
Fever: Instruct patients to monitor their temperature daily and notify the healthcare provider immediately if it reaches 100.4°F (38°C) or higher or the threshold specified by their physician.
Chills: May or may not accompany fever. It should be reported regardless.
Cold-like Symptoms: A runny nose, sore throat, and cough may indicate an emerging infection. Patients should document the onset of symptoms and notify their provider.
Body Aches: May signal viral illness, including influenza. Patients should report any generalized aching promptly.
Gastrointestinal Symptoms: Nausea, vomiting, or diarrhea can be dangerous due to fluid loss and the risk of sepsis. Immediate reporting is essential.
Changes in Mental Status: Especially in older adults, confusion or sudden changes in mentation may indicate an infection, such as a urinary tract infection, or even mimic stroke symptoms.
Urinary Symptoms: Pain, foul odor, or changes in frequency or appearance of urine should be reported.
Catheter Site Changes: Redness, pain, swelling, or discharge at catheter sites must be reported immediately. Use return demonstration to teach and evaluate proper catheter site care.
Vaginal Changes: Educate patients to report new vaginal itching, irritation, odor, or unusual discharge.
2. Daily Precautions and Hygiene
Hand Hygiene
Stress the importance of frequent handwashing with soap and water or alcohol-based hand sanitizers.
Emphasize critical times for handwashing: before eating, after restroom use, after returning from public spaces, and after touching pets or shared surfaces.
Use return demonstrations to assess understanding.
Oral Care
Instruct patients to brush their teeth twice daily with a soft-bristled toothbrush to avoid gum injury.
If tolerated, brushing after meals is also beneficial.
Skin Protection
Shaving: Use electric razors instead of blades to prevent cuts.
Footwear: Avoid going barefoot. Wear well-fitting shoes to prevent skin injury, blisters, or pressure sores.
Sun Exposure: Encourage protective clothing and hat use outdoors to avoid skin damage.
Wound Care: Any cuts, scrapes, or blisters should be cleaned immediately and covered with a clean, dry bandage.
3. Environmental and Social Precautions
Help patients understand how to reduce exposure to potential sources of infection:
Avoid Crowds: Instruct patients to avoid busy areas like malls, concerts, public transportation, and sporting events.
Avoid Sick Contacts: Limit contact with anyone showing signs of illness (fever, cough, sore throat, etc.).
Gardening: Soil can harbor harmful organisms; avoid gardening or wear gloves and a mask if necessary.
Pet Waste: Patients should not clean litter boxes or handle pet feces—delegate this task to others.
Public Mask Use: Encourage mask use in crowded or enclosed public spaces to reduce the risk of airborne infections.
Nursing Notes
This guide is not exhaustive, but it is a practical refresher and checklist for key patient teaching components. Nurses should:
Reinforce education consistently throughout the hospital stay.
Use return demonstrations and teach-back methods to confirm patient understanding.
Reference institution-specific educational materials and discharge protocols.
Document all teaching and the patient's level of knowledge before discharge.
(MD Anderson Cancer Center, 2024)
Oncology nurses can be found working in many different settings. With over 100 types of cancer, some may even subspecialize in a particular type, such as neurology, breast, or colorectal. A registered nurse or nurse practitioner can become certified in different areas, such as Oncology Certified Nurse (OCN), Certified Pediatric Hematology Oncology Nurse (CPHON), Certified Breast Care Nurse (CBCN), or an Advanced Oncology Certified Nurse Practitioner (AOCNP). More information can be found at the following website, https://www.oncc.org/, on these certifications and their requirements for sitting for the exam.
Even though some types of cancers are declining, the diagnosis will most likely never be eradicated. However, in the face of cancer's many challenges, it is often the compassion of nurses that brings light to the darkest moments. Their unwavering dedication, empathy, and strength not only support healing; they inspire it. As we celebrate Oncology Month, let us also take a moment to recognize the silent heroes beside the patients: the nurses who walk each step of that journey with care, courage, and compassion.
Working together, patients and nurses write stories of resilience, courage, and, above all, hope every day.
References
American Cancer Society, (2025, January 16). ACS Annual Report: Cancer Mortality Continues to Drop Despite Rising Incidence in Women; Rates of New Diagnoses Under 65 Higher in Women Than Men. https://pressroom.cancer.org/2025CancerFactsandFigures
American Society of Hematology. (2025). Blood basics. https://www.hematology.org/education/patients/blood-basics#:~:text=Blood%20is%20a%20specialized%20body,plasma%20and%2045%25%20blood%20cells.
MD Anderson Cancer Center. (2024). Patient education: Neutropenia. Retrieved from https://www.mdanderson.org/patient-education/Leukemia/Neutropenia.pdf
Subhan Waleed, M., Besa, E.C., da Costa Dourado, C.M., & Talavera, F. (2024). Neutropenic treatment and management. Retrieved from https://emedicine.medscape.com/article/204821-overview




Comments